Engineering New Tissue for Pediatric Heart Surgery
Unlike heart disease in adults, which typically develops over time, pediatric heart defects most often are present at birth. They are, in fact, the most common birth defect, affecting eight out of every 1,000 newborns, or more than 35,000 children annually in the United States, according to the National Heart, Lung and Blood Institute.
These include simple problems, which either need no treatment or easily can be repaired, as well as more complex structural ones, which often require multiple surgeries starting at birth.
It's these latter pediatric heart problems that preoccupy Jeffrey Jacot, assistant professor of bioengineering at Rice University and Texas Children's Hospital. The National Science Foundation- (NSF) funded scientist is designing new tissue engineering approaches with the aim of making pediatric heart surgery less invasive, possibly even unnecessary.
Jacot is not a physician, but works alongside surgeons and other health professionals to create novel new therapies for young patients with heart disease.
One aspect of Jacot's research involves using stem cells from an infant's own amniotic fluid to generate natural heart tissue that he hopes will vastly improve upon the synthetic patches currently used in heart repair. "Our goal is to be able to grow such tissue in the lab that can restructure the geometry of the heart," he says. "We hope it could replace successive surgeries, and lead to long-term good outcomes, and possibly a complete cure."
The artificial patches must be replaced as a child grows, whereas, if successful, the bioengineered tissue "will grow along with the patient and be functional tissue, not just a piece of plastic in the heart," Jacot says. "There won't be a rejection problem, since it's the infant's own amniotic fluid, and there won't be a need for successive surgeries."
Amniotic fluid is the protective liquid that surrounds the fetus during pregnancy, and research already has shown that it is a rich, natural source of stem cells. Stem cells have the ability to develop into many different cell types in the body, and also serve as an internal repair system, dividing essentially without limit to replenish other cells.
When a stem cell divides, each new cell has the potential either to remain a stem cell or to become another type of cell with a more specialized function, for example, a muscle cell, red blood cell, brain cell--or, in this case, a cardiac cell.
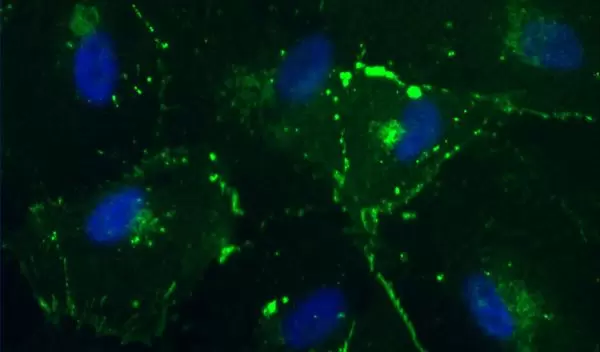
Jacot currently is focusing on how to grow these cells and regenerate them, and already has been able to isolate stem cells from human amniotic fluid. The hope is that these cells will have more potential than adult stem cells to differentiate into more specific types of cells, such as heart cells.
"This involves adding the right growth factors at the right times, to turn on the expression of specific proteins and transcription factors that will turn on the expression of other genes," he explains. "We are trying to figure out what populations of cells are in this amniotic fluid, and what are the best ones to respond to these growth factors and have the potential to become cardiac cells."
The researchers also are studying blood vessels that go through the heart, "knowing that any patch we make will have to have a blood supply," and already have created endothelial cells--cells that line blood vessels--from the same stem cells isolated from amniotic fluid.
"So, essentially, you are taking the same cells and using them for two different purposes," he says. "Both will go into making cardiac engineered heart tissues, but we turn them into different cell types."
Jacot's endothelial cell work was published last June in Tissue Engineering.
Jacot is conducting his research under an NSF Faculty Early Career Development (CAREER) award, which he received in 2011. The award supports junior faculty who exemplify the role of teacher-scholars through outstanding research, excellent education and the integration of education and research within the context of the mission of their organization. NSF is funding his work with about $450,000 over five years.
There are at least two complex pediatric heart defects that potentially could benefit from his work.
Humans are born with a four-chambered heart that includes two ventricles, one on the right and one on the left. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen-rich blood from the lungs and pumps it to the body.
"Every year about 1,000 infants are born with a single ventricle; either they don't separate or one doesn't develop," Jacot says. "An infant can't survive with this condition. Very shortly after birth, the vessels that connect the lungs to the rest of the body will close off, so there needs to be an operation very quickly after birth."
Another commonly occurring defect, the most common complex pediatric heart defect, is called tetralogy of Fallot, a combination of several structural abnormalities which results in insufficient blood supply to the lungs and, consequently, oxygen-poor blood flow to the rest of the body. This occurs in nearly four of every 10,000 live births, according to the Centers for Disease Control and Prevention.
Both conditions may require multiple surgeries as children grow. Even with the operations, the youngsters "will have much more limited function and a much higher chance of heart failure," Jacot says. "Their activities must be curtailed. The only complete cure now is to do a transplant, and pediatric organs are somewhat scarce."
Jacot thinks it may be possible, using bioengineering techniques, to substitute a patient's own tissue, grown from stem cells, for plastic patches now used, and even possibly, in the case of a child born with only one ventricle, build an extra ventricle from the material, "which can't be done now."
Currently, in the latter case, "surgeons will do a single ventricle repair, enabling it to deliver blood to both the lungs and the rest of the body," he says. "It has a good success rate, but it becomes inadequate after about a year. It's not enough to supply a growing child's needs, so they have to go back and do a second surgery, and successive surgeries after that."
Many such heart defects can be detected through a routine ultrasound during the second trimester. After discovering a defect, physicians typically conduct an amniocentesis, where they collect amniotic fluid for further examination to look for specific related genetic abnormalities.
"This gives us a unique opportunity to create lab grown tissues from the cells we get from the amniotic fluid at the time the defect is detected," Jacot says. "So the cells will be available, and getting them won't pose any added risk. We then will have months of time to expand those cells in the laboratory, to make them into the right cells for heart tissue and grow them, so that by the time the infant is born, there is a piece of heart tissue genetically matched to that infant."
Surgeons, then, will have a piece of the child's own tissue to use in structurally repairing the heart. "We think there is a very good chance of therapies like this succeeding," he says. "Everything is coming together now in terms of understanding how these cells grow, and how heart tissue develops."


