Wildlife species provide clues to spread of antibiotic resistance in Africa
Find related stories on NSF's Environmental Research and Education (ERE) programs at this link.
Antibiotics are a blessing that can also become an empty promise when microbes grow stronger and become resistant to the arsenal of modern medicine.
Globally, the emergence of antibiotic resistance is an important threat to human and other animal health. Monitoring resistance in wildlife can help, scientists say.
Differences in lifestyles among species can provide critical insights into the mechanisms of antibiotic spread, researchers report in the current issue of the Journal of Wildlife Diseases. NSF supported the study.
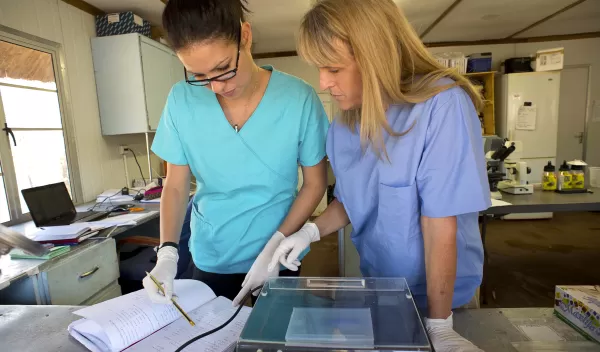
Researchers Kathleen Alexander of Virginia Tech and Sarah Jobbins of the University of Sydney tested for resistance to 10 antibiotics among 18 wildlife species and cattle in Chobe, Botswana. Alexander is also affiliated with the Centre for Conservation of African Resources: Animals, Communities and Land Use in Botswana.
Keys to resistance
The biologists explored key attributes and behaviors that may increase exposure and allow resistance to move between humans, other animals and ecosystems.
They compared results among 193 human samples from healthy and clinically ill patients at a local hospital, and with 12 environmental sources of human fecal waste.
The researchers used the common intestinal bacteria E. coli to evaluate antibiotic resistance exposure in humans, domestic animals and wildlife communities in northern Botswana. Among 150 wildlife samples, 41 percent contained E. coli isolates that were resistant to at least one or two of the 10 antibiotics tested, while 13 percent were resistant to three or more--and considered to be multi-drug resistant.
"It has only recently become apparent that antibiotic-resistant microbes have spread well beyond the human population into wildlife populations, but the mechanisms by which this happens have been unclear," said Alan Tessier, acting director of NSF's Division of Environmental Biology, which funded the research through NSF's Dynamics of Coupled Natural and Human Systems (CNH) Program.
NSF's CNH Program is supported by its Directorates for Biological Sciences, Geosciences, and Social, Behavioral & Economic Sciences.
"These results show that habitat use and a species' position in the food web are linked with antibiotic resistance," Tessier said.
Sampling results
E. coli from wildlife, human and environmental samples were resistant to a similar spectrum of antibiotics--ampicillin, doxycycline, streptomycin, tetracycline and trimethoprim-sulfamethoxazole.
Multi-drug resistance was found across land types, from areas of human habitation to protected areas such as national parks.
"Resistance was widespread but not ubiquitous, and isolates from wildlife demonstrated similar patterns of resistance to human E. coli from environmental and clinical sources in the study area," said Jobbins.
Multi-drug resistance was significantly higher in water-associated species such as hippopotamus and otters; carnivores such as crocodiles, leopards and hyenas; and species inhabiting urban areas such as baboons and warthogs.
Surface water is a critical shared resource for humans and other animals, particularly in dry regions of the world such as Botswana.
Aquatic life
Aquatic or semi-aquatic animals, such as crocodiles, otters and waterbucks, harbored significantly greater levels of multidrug-resistant E. coli, said Jobbins.
"But consumption of water alone was not the driver here," she said. "Several water-dependent species, such as impala, buffalo, cattle and sable, had little or no evidence of exposure to antibiotic resistance. These findings suggest that the duration of exposure and consumption of water-inundated vegetation and sediment might be the key to exposure and transmission of resistant microbes."
Multi-drug resistance was significantly higher in carnivores, animals at the top of the food chain that might have greater exposure to antibiotic resistance through diet.
Broad range of study
Jobbins and Alexander's study, they said, is one of the few to examine antimicrobial resistance in a broad range of hosts in their natural environment.
"This novel approach may be applied to other ecosystems, facilitating early detection of antimicrobial resistance accumulation in the environment," said Alexander.
The researchers concluded that long-term monitoring of antimicrobial resistance among top predators and water- and human-associated species may help in detection and control of the spread of antimicrobial resistance.
"Wildlife communities provide a unique opportunity for us to understand how antimicrobial resistance moves across landscapes," said Alexander.
"Each species occupies a particular niche and interacts with the environment in specific ways, dependent on key life history strategy elements. Wildlife communities may provide clues to points where humans, animals and natural systems are coupled and the transmission of antimicrobial resistance is occurring."
Global concern
The presence of antibiotic resistance is of grave concern, Alexander believes.
"This is an emerging problem of global proportions, resulting in failed treatments and deaths," she said.
With one of the highest rates of HIV/AIDS in the world, Botswana is extremely vulnerable to infectious diseases.
"Alarmingly, our research identifies widespread resistance in wildlife to several first-line antimicrobials used in human medicine," Alexander said. "In an environment where there are no commercial agriculture or livestock production activities, our next step is to establish why we are seeing these patterns."


