Scientists Use Math to Build Better Stents
Suncica "Sunny" Canic was good at math in school, so that's what she pursued as a career. But she always liked medicine, too.
When she moved to Houston, Texas, and met some cardiologists at a party, she started talking with them about what they do--and knew she could help.
"I realized we could provide them with a fluid dynamics and mechanics point of view to help them make decisions ... for example, about which stent grafts they use in their procedures," she said.
Stents are tiny mesh tubes made from metal alloys that hold blood vessels open after they've been clogged with disease-causing plaque. Even though stents are designed to be compatible with the human body, they sometimes cause unwanted reactions, such as blood clots and scar tissue formation. So, scientists have tried to coat stents with cells that make the tiny tubes even more compatible.
But these, too, aren't yet perfect, said Canic, a professor of mathematics at the University of Houston. Blood flowing over a coated stent can still clot or tear cells away. This is, as Canic put it, "not good." Supported by a joint grant from the National Science Foundation (NSF) and the National Institutes of Health's National Institute of General Medical Science (NIH/NIGMS), Cancic makes computer models to guide the search for a better stent coating.
She also uses computer models to study the strengths and weaknesses of different stent structures. Her work could help manufacturers optimize stent design and help doctors choose the right stents for their patients, ultimately improving patient outcomes.
Computer scientists usually model stents in three dimensions. Keeping track of about 200,000 points, or nodes, along the stent mesh, the models are massive.
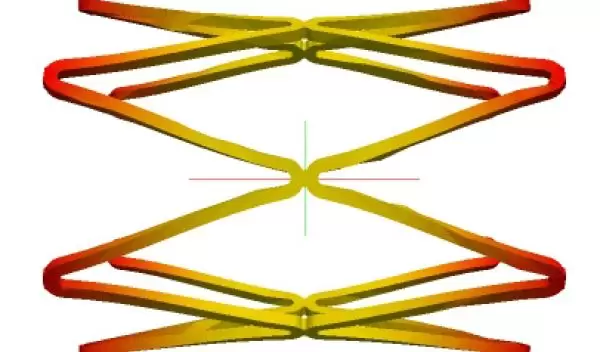
Together with her collaborator, Josip Tambaca of the University of Zagreb in Croatia, and her doctoral student, Mate Kosor, Canic wrote a much simpler program that approximates stents as meshes of one-dimensional rods. This program let the researchers achieve the same result using just 400 nodes.
Using their simplified model, the researchers have examined the designs of several stents on the market to see which structures seem to be best for specific blood vessels or procedures. For instance, they found that stents with an "open design"--where every other horizontal rod is taken out--bend easily, which makes them good to put in curvy coronary arteries.
Canic and Tambaca have also used the model to design a stent with mechanical properties specifically tailored to an experimental heart-valve replacement procedure. She found that this specialized stent works best for the procedure when it's stiff in the middle and less stiff at the ends. In addition, she has found that combining "bendiness" with radial stiffness--where you can bend the stent into a U shape, but you can't squeeze the tube shut--produces a stent with less chance of buckling than those that are currently in use.
The most rewarding part of her work, said Canic, is that "we can use mathematics for something useful, connected to real-world problems." She reports that her collaborators are already putting the results of her simulations into practice.
Meanwhile, her greatest challenge is serving as an ambassador of mathematics to the medical and bioengineering communities.
In the beginning, she said, it was difficult to collaborate with people from different disciplines who speak different scientific languages. "But once they saw that there is a lot of information there that could be helpful, it has been much easier," she said. "Now people want to talk to us from the medical center. They come to us and ask questions, and that's good."
Today, Canic is helping a team at the Texas Heart Institute study an unusual source for stent coating: ear cartilage. The team believes this easy-to-harvest tissue will make stents more biocompatible, though they don't yet know how ear cartilage cells grow or behave in environments like human blood vessels.
Canic is using her computer programs, developed together with Tsorng-Whay Pan, Roland Glowinski and students, to simulate how blood interacts with the stent-coating cartilage cells and how the cells stick (or don't) to the stent surface. She plugs in different fluid thicknesses and shear forces of blood flowing over the stent to see what might encourage the cartilage on freshly coated stents to stabilize quickly. The models have helped her collaborators learn the best conditions to test in follow-up experiments as they search for ways to pre-treat stents before doctors implant them.
Canic wants to keep collaborating with the medical community as she moves forward with her research. She plans to look at biodegradable stents, as well as simulating the fluid dynamics of regurgitating mitral valves (where some blood flows backwards in the pumping heart) to help doctors more accurately diagnose the condition using ultrasound. "Certainly, I am going to continue working in this area," she said. "It is very rewarding."
-- Stephanie Dutchen, NIGMS/NIH, stephanie.dutchen@nih.gov
This Behind the Scenes article was provided to LiveScience in partnership with the National Science Foundation.


